Bladder cancer latest treatment
How is bladder cancer treated?
There are so many different types and stages of
bladder cancer that therapy varies widely among individual patients. A single papillary tumor may be successfully treated by electrically destroying the tissue. When the tumor is
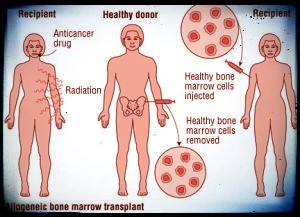
malignant and extensive, it may be necessary to remove the entire bladder. Multiple tumors, even at an early stage, are usually treated by surgical removal of the tumors themselves as well as surrounding tissue. Following surgery, a solution containing an anticancer drug may be instilled into the bladder to decrease the chance of the tumors recurring. If surgery is not available, radiation therapy can be used to destroy the cancer.
Tumor killing doses of
radiation can be delivered to the bladder without excessive damage to overlying tissues, permitting the cure of some advanced tumors not suited to surgical removal. Radioisotopes and
chemotherapy are also used in the treatment of bladder cancer. Sometimes radiation is used before the
operation in bladder cancer.
How is a diagnosis of bladder cancer made?
A urologist usually performs an examination with a cystoscope, which allows him to inspect the lining of the urinary bladder. If any suspicious looking areas or growths are observed, a piece of tissue is removed for microscopic examination without major surgery. The examination involves little time or discomfort. Cystograms, made after filling the bladder with an opaque solution, give further information about the size of the tumor and the width of its base. Intravenous pyelograms can be done to outline the ureters and upper urinary tract. Microscopic study (
cytology) of the urine for presence of
cancer cells sloughed off by the bladder is routine.
Understanding Bladder Cancer
What is a transurethral resection (TUR) and fulguration?
This is the removal of a bladder growth with electrical current. Using a cystoscope, which is passed through the urethra, the doctor removes the growth and burns out the surrounding tissue with electric current. It is most commonly used on small, benign growths. This is successful if only the superficial layer of the bladder has been invaded. After this treatment your doctor will ask you to return every 3 to 4 months, because new tumors have been known to grow in the same vicinity in about one quarter of all cases. If no recurrences are found after a year, the intervals between examinations may be lengthened gradually.
What surgical procedures are used if the cancer is more extensive?
Depending on where the cancer is located and how far it has advanced, the doctor will perform either a segmental resection or a cystectomy.
What is involved in a segmental resection?
A segmental resection is used only if the tumor is localized in one area of the bladder with an adequate margin of tissue that can be removed from around the tumor. This operation is performed through a lower abdominal incision and, when complete, the patient is left with a portion of the bladder and therefore can maintain urinary control. When this is not possible, then a cystectomy is necessary.
Bladder Cancer Latest Treatment Options
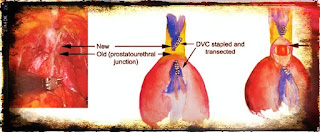
What is a cystectomy?
The operation for removal of the bladder is called a
cystectomy. In order to remove all the tissue containing the cancer safely and completely, it is sometimes necessary also to operate on other nearby parts of the body. In women, this may mean the removal of the ovaries, fallopian tubes, and uterus, as well as a portion of the vagina which contains the urethra. In men, the prostate and seminal vesicles may also be removed. If the tumor is near the opening of the bladder neck or involves areas of the bladder lining, the urethra may also be removed. A cystectomy is a major operation, but with modern surgical techniques and anesthetics, it can be carried out successfully.
Is radiation sometimes used before surgery?
Preoperative radiotherapy has been found to produce partial or even complete destruction of tumors of the bladder and is sometimes used before a cystectomy is performed.
How long will I remain in the hospital after my cystectomy?
Usually the recovery period lasts 2 or 3 weeks.
What anesthesia is used for bladder operation?
Usually spinal anesthesia is used. General anesthesia may also be recommended.
Where is the incision?
The incision begins in the midline, above the navel, and extends to the level of the pubic bone.
How long does the operation take?
This is a complicated operation which takes between 5 and 6 hours to perform.
How long will the stomach tube remain in place after surgery?
This tube, placed through your nose and into your stomach to drain the gastric juices and prevent accumulation of air and fluid in your stomach, usually remains in place after surgery for 5 to 7 days, until your bowels have regained normal activity. This will allow your stomach and bowels to rest and give the connection time to heal.
What special preparations are made before surgery?
Usually, you are admitted to the hospital a few days before the scheduled surgery. Daily enemas and laxatives will be given to you. In addition, you may be given antibiotics to reduce the amount of bacteria in your system. A special diet and vitamin supplements will be ordered for you. Your doctor or nurse may ask you to test a sample appliance to ensure that the area chosen for your stoma is on the flattest possible surface and provides maximum comfort for your various normal activities.
How is urine stored and emptied when one has had a cystectomy?
The surgeon removes a small section of the small intestine and converts it into a conduit, or pipeline, for urine. The ureters tubes that carry urine from each kidney to the bladder are joined to one end of the segment. The other end is brought out through the wall of the abdomen, near the navel, where it forms an opening called a stoma. A flat bag is placed over the opening to collect the urine. The bag is held to the body with a special type of glue.
Does this mean I'll have to wear a bag outside my body to collect the urine?
Yes. Though this is a large change in lifestyle, most patients find that they can adjust to the change once they understand that the existence of a stoma on the abdomen and a collection device over it need not be limiting or disabling. Hundreds of patients of all ages have had to face this adjustment and have found that they can handle it and resume normal activities.
Can I have a say in where the opening is placed?
Your doctor will usually discuss this with you, since the site should be determined before the operation. Generally it is located either in the right lower or upper abdomen. It should be placed where, when the collection appliance is attached, movements such as sitting, standing, twisting, and bending will not pull the appliance loose. It should not be located near an old scar or attached near rolls of fat. This should all be discussed with your doctor before the operation.
Will I be rigged to a urine collection device when I leave the operating room?
The temporary appliance will be placed over your stoma in the recovery room. This appliance will be connected to a continuous drainage bag that will be emptied of urine by one of the nurses or nurse's aides. For the first few days someone else will take care of you and your stoma. As you gain strength you will be taught how to do this yourself. It is important that you learn to care for your appliance and have confidence in it before you leave the hospital.
Is there any way I can try the appliance out before the operation?
Yes. The nurse can help you try out the appliance. She can apply it and put water in the pouch to simulate the weight of the urine. You can dress yourself and try doing some of your normal activities. This trial is a good way to eliminate your own anxieties about wearing the appliance. Keep in mind that there are many different types of appliances and many different solutions. You may need to try several before you find one that suits you.
How often should the appliance be emptied?
About every 2 hours.
What happens to the appliance during sleep?
Usually during sleep the appliance is connected to drainage tubing attached to a bottle placed on the floor beside the bed. Running the tubing under the leg allows greater freedom of movement. Most patients find they can sleep in any position once they are accustomed to wearing their appliances.
Does the urine look the same as before?
It does not look exactly the same as urine from the bladder, since the conduit through which it passes is made from a segment of the small intestine, which secretes mucus. This mucous membrane is sensitive, and urination can cause mucus as well as slight amounts of blood to appear in the urine. Check with your doctor if there are changes in the consistency or color of the urine or a decrease in the amount of drainage.
Should I get a spare appliance?
Yes. It is a good idea to have one to wear and one to keep ready for use. This ensures that the one to be applied will be well dried and aired. You'll find you need a new appliance about every 6 months.
Can I bathe and shower as usual?
Yes. You can bathe and shower with or without the appliance. If the stoma seems irritated, remove the appliance and soak yourself in a tub of warm water.
How does a cystectomy affect a man's ability to function sexually?
It depends upon the extent of the operation. Sometimes sexual function may be impaired even though the penis is left intact. You should discuss this point with your doctor before he performs the operation so that you will know how extensive the surgery will be.
Are women still able to function sexually?
Sexual activity may be possible, but it could be impaired if a portion of the vagina is removed. Again, this is a topic which you should discuss with your doctor before the operation is performed.
Is it usual for a patient to be depressed after this kind of operation?
It is not unusual to feel depressed. As a result of the depression, the patient's attention span may be short, and he or she may have difficulty in concentrating and be irritable. It is important for the family and friends to realize that this is a temporary but normal feeling. An inability to cope with the new way the body functions may reinforce the thought that the person may never be able to cope with anything again. The depression is usually short lived and subsides when the patient finds that family and friends accept him or her and that he or she can return to a normal way of life.




Comments
Post a Comment