How painful is a bone marrow transplant for the donor
What is a bone marrow transplant?
Bone marrow transplantation is an approach used over the past 10 years for the treatment of acute leukemia and lymphoma. It is a complex procedure and should be undertaken only by physicians with the experience and resources needed to get the best results.When is a bone marrow transplant used?
It may be used in some cases of several types of diseases aplastic anemia (when patients do not have enough red cells to carry oxygen, enough white cells to fight bacteria, or enough platelets to help clotting), in some types of acute and chronic leukemia, for some lymphomas, for severe combined immunodeficiency syndrome, and for certain inherited blood disorders such as thalassemia. A bone marrow transplant replaces a patient's abnormal or diseased marrow with healthy marrow from a donor.Can any leukemia patient undergo a bone marrow transplantation?
No. When patients and doctors consider the possibility of treatment with a bone marrow transplant, they must evaluate factors such as the patient's specific illness, age, and medical history; other treatments that might have been used earlier; and the possible risks and benefits of the transplant in the patient's particular case. Some types of leukemia and lymphoma, for example, are curable in many cases with anticancer drugs and/or radiation therapy. These treatments would be tried first, before bone marrow transplantation is considered.When is bone marrow transplantation considered as a possible treatment?
Bone marrow transplants are sometimes suggested for patients whose leukemia has failed to respond to other methods of treatment, primarily chemotherapy, or who have forms of disease which have been identified as resistant to treatment. Patients with acute lymphocytic leukemia, acute myelogenous leukemia, chronic granulocytic leukemia, and resistant forms of leukemia and lymphoma may be candidates for bone marrow transplants. There are many considerations in determining if a patient might benefit from a transplant, including age of the patient (usually, but not always, under 45), general physical health, condition of organs such as the heart and liver, and prior treatment for blood cell or other diseases.What questions should I ask my doctor about bone marrow transplants?
• Is a bone marrow transplant the best option for treatment of my condition?• What are the chances that the donated marrow will not grow in me?
• With my condition, what are my chances ofbeing cured?
• What are the risks and possible side effects of a bone marrow transplant?
• What is the cost of a marrow transplant and how does it compare with the cost of other possible therapy?
• How long will I have to stay in the hospital?
• How long must I be treated as an outpatient?
• What are some of the risks and side effects of the radiation and chemotherapy used to prepare me for transplantation?
• How soon after the transplant will I be able to resume normal activity?
• If the transplant is done, will I need other treatment?
• What kind of complications occur?
• Because of the risk of infection, can friends and family visit me in the hospital?
• After the transplant, how often will I need medical checkups?
What is a bone marrow transplant?
Who can donate bone marrow?
The ideal donor is an identical twin, because there is no risk that the patient will reject the graft. However, transplants are usually performed with marrow donated by other family members. Studies with animals have shown that a graft is more likely to take if certain proteins on the surface of white blood cells are the same for both the donor and the recipient. There is a 25 percent chance that any one brother or sister will have the same protein (HLA antigen) as the patient, since these proteins are inherited from the parents one set from the mother and one from the father.Are there different kinds of bone marrow grafts?
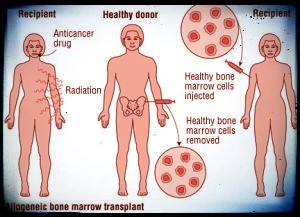
There are three different kinds. An autologous graft is taken from the patient's own marrow, removed before the patient is given chemotherapy or radiation. The marrow which is removed may be treated before it is retransplanted to the patient. A syngeneic graft comes from an identical twin. An allogeneic graft comes from a parent, brother, or sister.How is the patient prepared for the graft?
The patient is usually given a treatment radiation and a high dose of cyclophosphamide to keep the immune system from rejecting the foreign marrow. In addition the patient is also given high dose chemotherapy to destroy cancer cells in the marrow and elsewhere, plus radiation over the entire body to penetrate the bones and kill leukemia cells in the marrow.How is the bone marrow taken from the donor and given to the recipient?
In an operating room, with the donor under general or spinal anesthesia, marrow is taken from the pelvic bone with a needle and syringe. The procedure takes about 3 hours. The marrow is passed through stainless steel screens to break up particles and is then injected into the recipient. The marrow cells enter the general circulation and go through the blood to marrow cavities in the recipient's bones. The cells begin to grow in the marrow and produce new white blood cells, red blood cells, and platelets.Is it painful to donate bone marrow?
The needle puncture sites may be tender for up to a week. Some stiffness and difficulty in walking will last for a day or so, but the discomfort can be lessened through exercise. Donors are usually released the following day. Marrow cells are quickly produced by the body, and the amount removed will be replaced in 2 or 3 weeks.Bone Marrow Transplant Process Explained
How soon will the transplanted marrow begin to produce new blood cells?
The transplanted marrow may not begin producing new blood cells for 2 to 4 weeks or longer. The patient needs intensive supportive care. Infections must be prevented. Patients and visitors use face masks and hand washing to minimize exposure to bacteria. The patient is given antibiotics and sometimes is placed in the sterile environment of a laminar air flow room. The patient may receive granulocyte transfusions to help prevent infection and red blood cells to prevent anemia. Transfusions of platelets are often required to prevent uncontrolled internal or external bleeding. All blood products given to transplant patients are treated with radiation to inactivate lymphocytes from the donor which could cause an immune reaction against the patient. Adequate nutrition is another important factor, and many patients are given their nutrients through a feeding tube.How do the doctors know if the graft has taken?
A rise in the number of granulocytes and platelets is usually a sign that the graft has taken. Gene markers in the blood and cytogenetic studies are among tests used to confirm that the donor marrow is growing. About 5 weeks after the actual transplant, the patient is allowed to leave the hospital if he is eating enough and has a normal temperature and satisfactory blood tests. Patients are not usually allowed to return to work or school for 6 to 9 months after the transplant, because the immune system needs that long to recover, and patients are especially susceptible to infections.What research is being done in bone marrow transplants?
Many transplant teams around the world are investigating new techniques. They include using an unrelated donor, using specially prepared antibodies called monoclonal antibodies, using the patient's own bone marrow by first cleaning the removed bone marrow with monoclonal antibodies or anticancer drugs, and examining the possibility of establishing a donor bank to collect marrow samples from donors in the general population.What is splenectomy?
This operation involves the removal of the spleen. It is sometimes used in the treatment of leukemia, especially CML, or in lymphomas when the spleen enlarges and is responsible for destroying large numbers of normal blood cells.Spleen removal is performed under general anesthesia. The incision is usually made in the upper left abdomen and is about 8 inches long. Once removed, the spleen does not grow back, but since its normal functions are taken over by other body tissues, the absence of the spleen does not interfere with normal living. Cancer of the spleen is rare, but when it does occur a splenectomy is the usual treatment.



Comments
Post a Comment